Self-regulation is a crucial element of providing holistic sensory integration and sensory based therapy. But what exactly does it entail? I like the four components of self-regulation that Leah Kyupers, author of the Zones of Regulation, highlights:
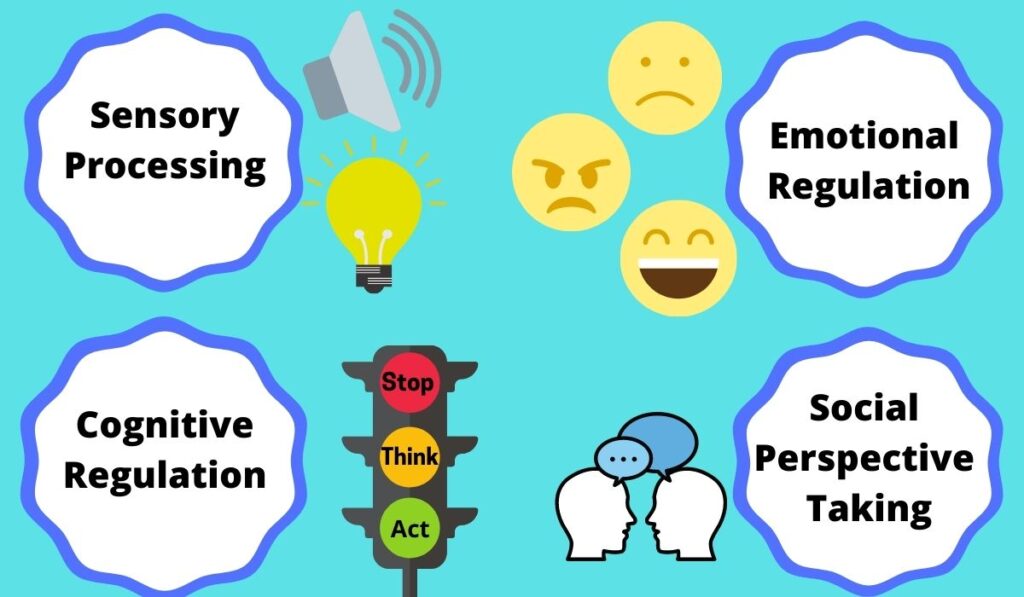
Part of the thought process behind implementing sensory integration and sensory-based therapy is that as a child’s sensory processing abilities improve, so too will their self-regulation. I think this definitely is a possibility, but we must be mindful that oftentimes the children we work with need to be directly taught regulation skills. As their sensory-processing improves, children may be more calm more of the time. This in turn may facilitate them learning self-regulation strategies for the next time they are becoming dysregulated. However, the need for direct modeling and practice of tools to regulate remains.
Journal American Journal of Occupational Therapy (SNIP score 1.121)
Article Title Effectiveness of Cognitive and Occupation-Based Interventions for Children with Challenges in Sensory Processing and Integration: A Systematic Review
- 1A Systematic review of homogenous RCTs
- 1B Well-designed individual RCT
- 2A Systematic review of cohort studies
- 2B Individual prospective cohort study, low quality RCT, ecological studies; and two-group, non-randomized studies
- 3A Systematic Review of case control studies
- 3B Individual retrospective case-control studies; one-group, non-randomized pre-post test study; cohort studies
- 4 Case series (and low quality cohort and case control study)
- 5 Expert opinion without explicit critical appraisal
- * This was a systematic review which included a wide array of evidence from RCT to Level IV single-case experimental design. As this type of systematic review doesn’t fall into either 2A nor 3A, I chose to categorize it into a level 2B study. The evidence reviewed was higher than case studies but lower than cohort studies.
Methods
The authors of this systematic review included peer reviewed studies that concentrated on interventions in the scope of OT for children and adolescents who had sensory processing and integration challenges. Authors of this review ensured this in that studies they included demonstrated the use of an assessment that specifically confirmed the participants had sensory processing or sensory integration challenges. The authors selected studies that also included outcome measures that specifically evaluated sensory processing and integration (Pfeiffer, Clark, & Arbesman, 2017, p. 3).
The authors of this review specifically reviewed interventions defined as either cognitive or occupation-based. I appreciate that the authors were specific by excluding studies that did not explicitly indicate subjects as having sensory processing or integration disorders (Pfeiffer, Clark, & Arbesman, 2017, p. 4) While it is sometimes frustrating to have less articles, it is better to have consistent and accurate definitions so that we can feel confident of what is being reported!
Findings
Two studies included evaluated cognitive interventions that targeted outcome measures of self-regulation and executive functions of inhibitory control, social cognition, behavioral and emotional regulation and externalizing behavior problems (Pfeiffer, Clark, & Arbesman, 2017, p. 5).
Alert Program for Self-Regulation
A level I study assessed the effectiveness of 12 individual 1 hour sessions of the Alert Program for Self-Regulation for children with Fetal Alcohol Syndrome. Authors grouped children into an immediate and delayed treatment group. The delayed treatment group served as the control. Both groups received treatment, with the group receiving treatment first demonstrating significant increases in their inhibitory control and social cognition. These gains were maintained at a 6 month follow-up. Also noteworthy is that parents of children in this group indicated their children’s behavior and emotional regulation improved. These parents also noted a reduction in externalizing behavior problems in their children (Pfeiffer, Clark, & Arbesman, 2017, p. 5).
Components of the Alert Program

Social Stories
A level IV study included an intervention of Social Stories for 9 weeks in a self-contained pre-school classroom. This intervention with 3 male pre-schoolers entailed reading and then talking about a Social Story concentrated on the children’s goals (Pfeiffer, Clark, & Arbesman, 2017, p. 5). Children also practiced their strategies as part of the intervention. The interventionists used Social Stories that met Carol Gray’s criteria for social stories.
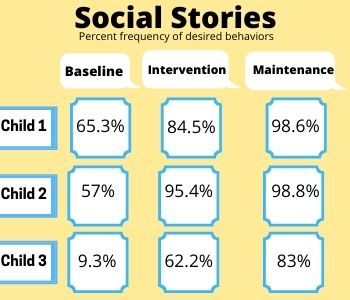
All three children in this study showed increased frequency of their desired behaviors. The baseline, intervention and maintenance phase percentages of frequency of desired behaviors are shown.
Occupation-Based Interventions
Horseback Riding to Promote Self-Regulation Skills
A level I RCT investigated the effectiveness of horseback riding on children’s social functioning. Subjects were children 4-10 years old with ASD. These children participated in 1 hour per week of horseback riding lessons for 12 weeks. This was done at an equestrian center with trained instructors. Children who participated in the horseback riding intervention demonstrated statistically significant changes in their overall Sensory Profile Score, as completed by their parents (Pfeiffer, Clark, & Arbesman, 2017, p. 6). Specifically, the following subscales were impacted: Sensory Seeking, Sensory Sensitivity, Inattention/Distractibility and Sedentary Behaviors. These children also demonstrated significant changes in social motivation.
A level III study used lessons that a school group coordinator designed about: sensory orientation to the environment, mounting a horse and riding (Pfeiffer, Clark, & Arbesman, 2017, p. 6). Subjects were children in kindergarten through fifth grade with ASD. Children who participated in horseback riding demonstrating significant improvements in their social interaction, sensory processing as well as reduced severity of symptoms associated with ASD. It is noteworthy that in this study, subjects had built in breaks and during breaks, the gains were not consistently maintained (Pfeiffer, Clark, & Arbesman, 2017, p. 6).
Yoga as a Means to Promote Self-Regulation
A level III study assessed the use of yoga for subjects 12-18 years old who were in partial hospitalization or an inpatient mental health unit (Pfeiffer, Clark, & Arbesman, 2017, p. 6). These subjects took part in at least two 50 minute yoga sessions over 5 months. A Yoga Alliance-registered teacher taught the classes. Participants in the yoga intervention demonstrated significant improvements in their pulse rate and self-reported distress ratings.
What’s the Best Way to Promote Self-Regulation?
As OT’s we know that there are many factors that contribute to our clients meeting goals and living fulfilling and enjoyable lives. I liked that this study highlighted both the need for cognitive strategies and occupations. Teaching children to become more aware of their body’s state of regulation helps empower them to self-regulate . I am excited to see that children can participate in occupations that are enjoyable that can also help develop self-regulation skills! What are your favorite programs and tools to teach children self-regulation?
References
Pfeiffer, B., Frolek Clark, G., & Arbesman, M. (2017). Effectiveness of cognitive and occupation-based interventions for children with challenges in sensory processing and integration: A systematic review. American Journal of Occupational Therapy, 72, 7201190020. https://doi.org/10.5014/ajot.2018.028233.